Bone Grafting
An Overview
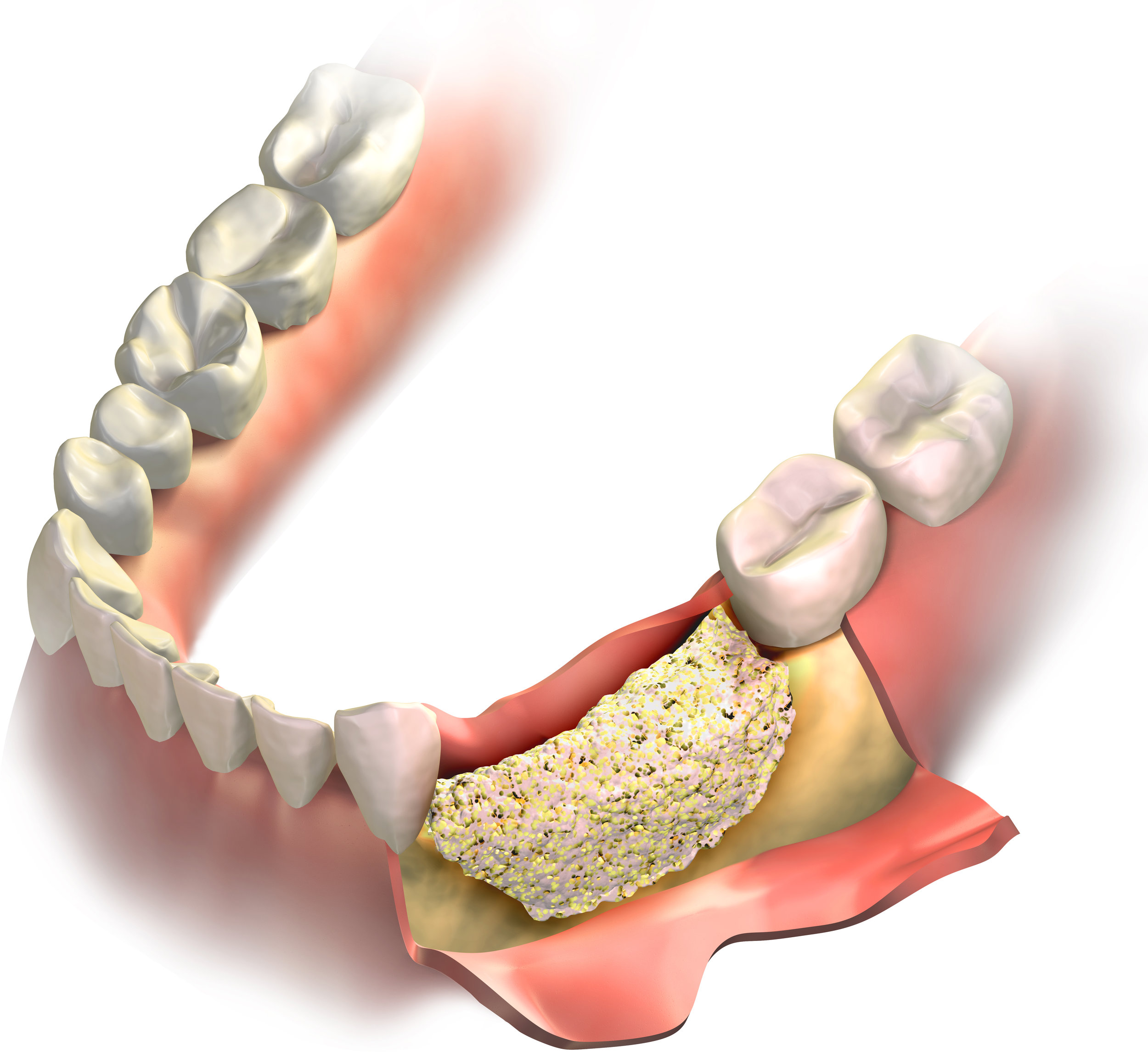
When a tooth is removed, the jawbone associated with that tooth collapses. This often leaves poor quality and quantity of bone needed for placement of dental implants.
Today, we can regrow that lost bone. This not only gives us the opportunity to place implants of proper length and width, it also gives us a chance to restore functionality and esthetics.
Bone grafting can repair potential implant sites with inadequate bone structure due to previous extractions, gum disease or injuries. The bone is typically obtained from a tissue bank, or in some cases from inside the mouth. In addition, special barrier membranes may be utilized that protect the bone graft and encourage bone regeneration. This is called guided bone regeneration (GBR). Sinus bone grafts are also frequently performed to replace bone in the posterior upper jaw.